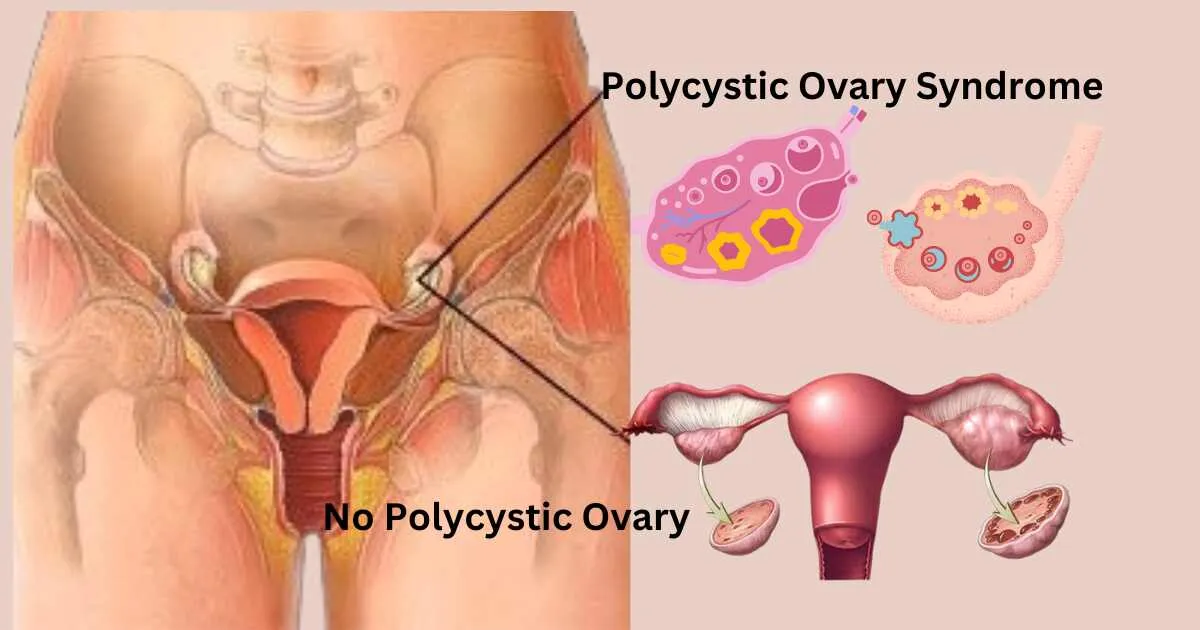
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder among women of reproductive age, affecting approximately 1 in 10 women worldwide. It is characterized by irregular periods, excess androgen levels, and polycystic ovaries. While PCOS is primarily known for its reproductive implications, its impact extends beyond physical health to mental well-being.

Introduction to Polycystic Ovary Syndrome (PCOS)
PCOS is a complex endocrine disorder characterized by hormonal imbalance, which can lead to various symptoms such as irregular periods, acne, and infertility. While the exact cause of PCOS remains unknown, factors like genetics, insulin resistance, and inflammation are believed to play a role.
Symptoms of PCOS
Women with PCOS may experience a range of symptoms, including irregular menstrual cycles, excessive hair growth (hirsutism), acne, and weight gain. These symptoms can vary in severity and may affect both physical and emotional well-being.
Link Between PCOS and Mental Health
Research indicates a strong correlation between PCOS and mental health disorders such as depression, anxiety, and eating disorders. Women with PCOS are at a higher risk of developing these conditions compared to those without the syndrome.
PCOS and mental disorders
Estrogen appears to have an effect as an antipsychotic. When levels drop too much, it becomes easier for psychological symptoms to emerge. For example, a number of reviews show that, in women with very chronic mental illness, their symptoms increase after childbirth, before menstruation, and during menopause.
Therefore, PCOS women may be more vulnerable to psychosis. Because they are exposed to high levels of unopposed estrogen for too long as a result of low ovulation. When they ovulate, they experience a sharp drop in their estrogen, which mimics the postpartum period. This may explain the susceptibility of women with PCOS to psychological symptoms.
Women with psychosis are more likely to have menstrual irregularities or amenorrhea, which is caused by hyperprolactinemia induced by the use of antipsychotic medication. Hyperprolactinemia can also greatly interfere with their ability to reproduce, which can be a major problem for the 71 to 72% of women with PCOS.
Antipsychotic medications have their negative impact on personal appearance causing associated weight gain, hair loss, acne, dental problems, halitosis, alopecia, rashes, tremors, stiff gait, very unsightly mouth, etc. Their actions, voice changes, and similar symptoms are associated with PCOS. Leading to negative body image, low self-esteem, perceived stigma. And high prevalence of anxiety and depression.
The high degree of overlap and overlap of symptoms between the two conditions may prevent identification of primary PCOS in psychiatric patients. Moreover, for women suffering from both the conditions, all these symptoms become very severe.
Understanding Mental Health Disorders Associated with PCOS
Depression and anxiety are among the most common mental health issues observed in women with PCOS. The hormonal imbalances and physical symptoms associated with PCOS can contribute to feelings of low self-esteem, stress, and mood disturbances.
Factors Contributing to Mental Health Issues in PCOS
Several factors contribute to the increased risk of mental health disorders in women with PCOS, including hormonal imbalances, insulin resistance, and body weight fluctuations. These factors can exacerbate existing psychological symptoms and impact the overall quality of life.
Impact of PCOS on Quality of Life
PCOS can have significant implications for a woman’s quality of life, affecting various aspects such as relationships, work, and self-image. The psychological distress associated with PCOS can lead to social isolation, impaired functioning, and reduced overall well-being.
Importance of Addressing Mental Health in PCOS
Recognizing and addressing the mental health aspect of PCOS is crucial for comprehensive management and improved outcomes. Integrating mental health support into PCOS treatment plans can lead to better symptom management and enhanced overall quality of life.
Strategies for managing mental health in PCOS
Managing mental health in PCOS requires a multifaceted approach involving lifestyle modifications, psychological support, and, in some cases, medication. Adopting healthy coping mechanisms, seeking therapy, and maintaining a balanced lifestyle can help alleviate symptoms and promote mental well-being.
Seeking professional help
It’s essential for women with PCOS to seek professional help from healthcare providers experienced in managing the syndrome and its associated mental health issues. Consulting a gynecologist, endocrinologist, or mental health professional can provide tailored treatment options and support.
Self-Care Tips for Improving Mental Health
In addition to professional support, self-care practices play a vital role in managing mental health in PCOS. Engaging in activities that promote relaxation, practicing mindfulness, and prioritizing self-care can help reduce stress and improve overall emotional resilience.
Support networks and resources.
Joining support networks and accessing reliable resources can provide valuable emotional support and practical guidance for women with PCOS. Online communities, support groups, and educational resources offer opportunities for connection, validation, and empowerment.
Conclusion of Polycystic Ovary Syndrome and Mental Health
PCOS not only affects reproductive health but also has significant implications for mental well-being. By recognizing the link between PCOS and mental health and implementing strategies for support and management, women can improve their overall quality of life and well-being.
FAQs
- Can PCOS medication help with mental health symptoms?
- While PCOS medication primarily targets hormonal imbalances, some women may experience improvements in mental health symptoms as a result of symptom alleviation.
- How can diet and exercise impact mental health in PCOS?
- A balanced diet and regular exercise can help manage weight, improve insulin sensitivity, and positively impact mood and overall mental well-being in women with PCOS.
- Are there any alternative therapies for managing mental health in PCOS?
- Some women find alternative therapies such as acupuncture, yoga, and meditation helpful in managing stress and improving mental well-being alongside traditional treatment approaches.
- Can PCOS ovaries cause mental health issues?
- Yes, PCOS ovaries can contribute to mental health issues due to hormonal imbalances and associated symptoms.
- Does PCOS affect personality?
- PCOS can affect personality indirectly through its impact on mental health and emotional well-being.
- Does PCOS cause anger issues?
- While PCOS itself doesn’t directly cause anger issues, the stress and hormonal fluctuations associated with the condition may contribute to mood disturbances.
- Can polycystic ovary syndrome affect your brain?
- Yes, polycystic ovary syndrome can affect the brain, primarily through its influence on hormone levels and associated symptoms such as mood swings and cognitive changes.




